We understand the same key does not fit every lock. This drives our philosophy to take customer service out of the box and craft our service around the needs of our clients. We make the effort to unlock the full potential in what we can do for you.
Both full and ongoing dependent eligibility verification and audit services are available. We collect, manage and validate legitimate Dependents and Qualified Life Event’s to save you time and money. On average clients experience a 5% – 8% total benefit cost savings!
Our dependent verification and eligibility audit process consists of 4 phases designed to educate employees about your plan’s eligibility rules, help prevent simple enrollment errors and future fraud and abuse.
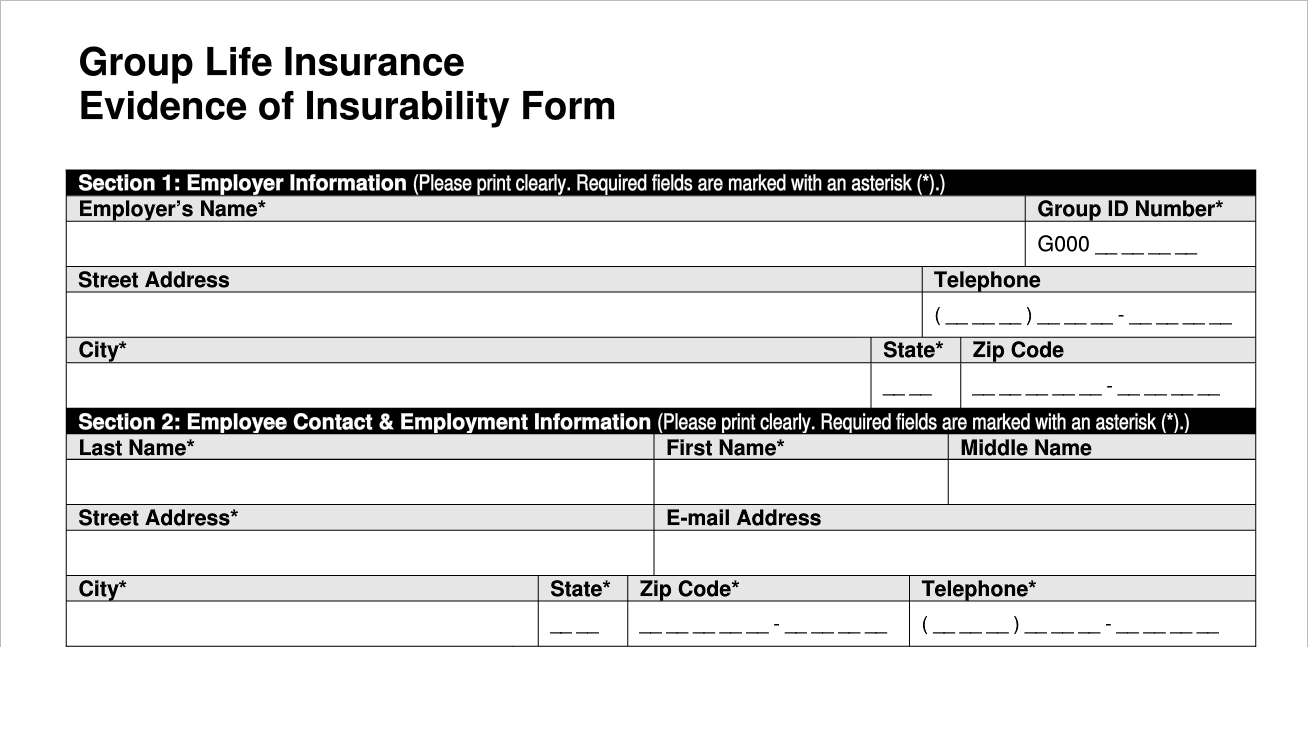
EOI administration service is available to process approved/denied carrier decisions to help our clients free up their time. This service is customized to fit your needs.
- EOI forms are collected, analyzed and processed according to the client’s wishes.
- Online employee records are updated and adjusted in accordance with the effective date and allowed or denied Insurance plan value(s).
- Notes are recorded in the employee’s online file.
"A customer is the most important visitor. (S)He is not dependent on us. We are dependent on him. He is not an interruption in our work. He is the purpose of it. He is not an outsider in our business. He is part of it. We are not doing him a favor by serving him. He is doing us a favor by giving us an opportunity to do so."
Mahatma Gandhi
- Dedicated in-house call center service is available at multiple levels to assist in on-line and real-time system training, open enrollment, initial enrollment, qualifying life events, special enrollment needs, HR Administrative and Employee help center needs, and for dependent verification services.
- All calls are recorded for playback and notes on the calls are kept on the employee’s secure record.
- Benefit Resource offers Email communication tracking. Records are kept for up to three years.
- We support fax and US Postal Service mail options.
- All issues are documented and tracked using Team Foundation Server, a 3rd party workflow software available through Microsoft.
"Fast is fine, but accuracy is everything."
Wyatt Earp
- Thorough data cleansing and preparation ensures consistency and data integrity. Client specific data gathering spreadsheets are used to assemble and analyze critical implementation elements. This is reconciled with election information to identify and manage variances.
- Demographic and election files are initially collected, analyzed and scrubbed to identify and manage pre-existing line item discrepancies.
- Benefit plan rules and rates are evaluated and reconciled against initial election files to ensure plan compliance and uniform translation into the Benefit Resource database.
- Full carrier files are accepted and used to facilitate line item comparisons.
- Standard on-demand discrepancy (error) reports are available.
- Ongoing and/or periodic carrier reconciliation is available.